Inflammatory bowel disease, also called IBD, represents a group of intestinal disorders causing prolonged inflammation of the digestive tract. Our digestive tract comprises the mouth, esophagus, stomach, small intestine, and large intestine. Its job is to break down food, extract the nutrients, and remove any unusable material. Inflammation that happens along the digestive tract disrupts this process, causing pain, and in some cases, may even be life-threatening.
IBD is actually an umbrella term that is used to describe a disease involving chronic inflammation of the digestive tract. So, what are the different types of inflammatory bowel disease?
Two major types of inflammatory bowel disease are Crohn’s disease and ulcerative colitis. Crohn’s disease involves any part of the gastrointestinal tract from the mouth to the anus. It is characterized by inflammation of the lining of your digestive tract which usually spreads deep into the affected tissues. Ulcerative colitis, on the other hand, is limited to the colon or large intestine. It can cause inflammation and sores (ulcers) in the innermost lining of the colon and rectum that can be long-lasting.
If you want to learn more about Crohn’s disease and ulcerative colitis, the symptoms, causes, and treatments. Keep reading!
What is Crohn’s disease?
Crohn’s disease is a type of inflammatory bowel disease that causes inflammation of your digestive tract, which may lead to abdominal pain, fatigue, weight loss, severe diarrhea, and malnutrition. It can affect all parts of your gastrointestinal (GI) tract, from the mouth all the way down to the anus. However, it may only affect some parts of the gastrointestinal tract and skip other parts. In some people, the disease only affects the last segment of the small intestine. In others, the disease is confined to the colon. The disease most commonly happens in the colon and the small intestine.
The inflammation that Crohn’s disease caused often spreads deep into the layers of the affected tissues. The disease can be both debilitating and painful. Sometimes, it may even lead to complications that are life-threatening.
Causes of Crohn’s disease
The exact cause of Crohn’s disease is still unknown. Diet and stress were suspected as the cause, but doctors now know that these factors do not cause the disease although they may worsen it. It is likely that a malfunctioning immune system and heredity play a role in the development of Crohn’s disease.
- Heredity – Crohn’s disease is more common in people who have family members with the disease. Up to 20% of people with the disease also have a parent, sibling, or child who has it.
- Immune system – a bacterium or virus that may trigger Crohn’s disease. In some cases, when your immune system tries to attack a virus or bacterium, it attacks your digestive tract as well.
Several factors are also found to increase your risk of developing the disease. These risk factors include:
- Family history – if you have a close relative with the disease, you are at a higher risk.
- Ethnicity – the disease can affect any ethnic groups, but whites have the highest risks, including people of Eastern European (Ashkenazi) Jewish descent. In recent years, more and more blacks who live in the United Kingdom and North America develop the disease.
- Age – while the disease may occur at any age, it is more likely that you develop the condition when you are young. Most people with Crohn’s disease are diagnosed before they are 30.
- Environment – your environment and where you live can be a risk factor. If you live in an industrialized country or in an urban area, it is more likely for you to develop the disease. This shows that environmental factors, such as a diet high in refined foods or fat may have a role in the development of the disease.
- Cigarettes – the most important controllable risk factor of Crohn’s disease is cigarette smoking.
- Nonsteroidal anti-inflammatory medications – medications, such as ibuprofen (Motrin IB and Advil, diclofenac sodium (Voltaren), naproxen sodium (Aleve), and others may lead to inflammation of the bowel, making Crohn’s disease worse.
Symptoms of Crohn’s disease
The signs and symptoms of Crohn’s disease can range from mild to severe. The symptoms usually develop gradually, with some symptoms may become worse over time. Although it is possible, it is rare for symptoms to develop suddenly and without wanting. It is also possible that you have no signs or symptoms for a certain period of time (remission).
The earliest symptoms may include:
- Abdominal cramps
- Diarrhea
- Blood in your stool
- Fatigue
- Loss of appetite
- A fever
- Weight loss
- Feeling a frequent need for bowel movements
- Feeling as if your bowels are not empty after a bowel movement.
As these symptoms can be similar to the symptoms of other conditions, such as food poisoning, allergy, or an upset stomach, it is possible to mistake them. If any of the above symptoms persist, you should see a doctor.
As the disease progresses, the symptoms may become more severe. More severe symptoms can include:
- Ulcers that may occur anywhere on the gastrointestinal tract, from the mouth to the anus
- A perianal fistula, which may cause pain and drainage near the anus
- Shortness of breath or decreased ability to exercise because of anemia
- Inflammation of the liver or bile ducts
- Inflammation of the joints, eyes, and skin
- In children, delayed growth or sexual development.
Early diagnosis can help you avoid severe complications and begin treatment early.
Complications of Crohn’s disease
Crohn’s disease can lead to one or more complications, including:
- Fistulas
- Bowel obstruction
- Ulcers
- Anal fissure
- Malnutrition
- Colon cancer
- Other problems, such as anemia, osteoporosis, skin disorders, arthritis, as well as gallbladder or liver disease.
Diagnosis and Treatment of Crohn’s disease
A combination of tests is used to confirm a diagnosis of Crohn’s disease, including blood tests, colonoscopy, CT scan, MRI scan, capsule endoscopy, and balloon-assisted enteroscopy.
There is currently no cure for Crohn’s disease. However, it can be well managed for a variety of treatments. These treatments can lessen the frequency and severity of your symptoms. The treatments include:
-
- Medications
There are several types of medications to treat Chron’s disease. The most commonly used are anti-inflammatory and anti-diarrheal drugs. More advanced options are biologics, which treats the disease using your body’s immune system. The type of medications you need depends on your symptoms, the severity of your condition, your disease history, and how you respond to treatment.
- Anti-inflammatory drugs – doctors use two types of anti-inflammatory drugs to treat Crohn’s disease, including corticosteroids and 5-aminosalicylates. Anti-inflammatory drugs are usually the first drugs you take as your treatment. These drugs are often recommended when you have mild symptoms.
- Immunomodulators – the inflammation leading to the symptoms of Crohn’s disease may be caused by an overactive immune system. Immunomodulators are drugs affecting the immune system. It can limit your immune system’s reaction and reduce the inflammatory response.
- Biologic therapies – a number of biologic therapies may be used to treat the inflammation and complications that occur from the disease. Biologic drugs are used to block specific proteins that may trigger inflammation.
-
- Dietary changes
While food does not cause Crohn’s disease, it can trigger flares. Your doctor may suggest you see a registered dietitian, who will help you understand how food can affect your symptoms and the diet changes that may help you. You may be asked to keep a food diary, which details what you ate and how it made you feel. The information from the food diary will help your dietitian to create eating guidelines. The diet that your dietitian gives will help you absorb more nutrients, as well as limiting any negative side effects that food may cause.
-
- Surgery
If dietary changes and less invasive treatments cannot improve your treatments, your doctor may recommend surgery. About 75% of people with the disease will require surgery. There are numerous surgery types. Some types of surgery involve removing a damaged portion of the digestive tract and reconnects the healthy sections. Other types manage scar tissue, repair damaged tissue, or treat infections.
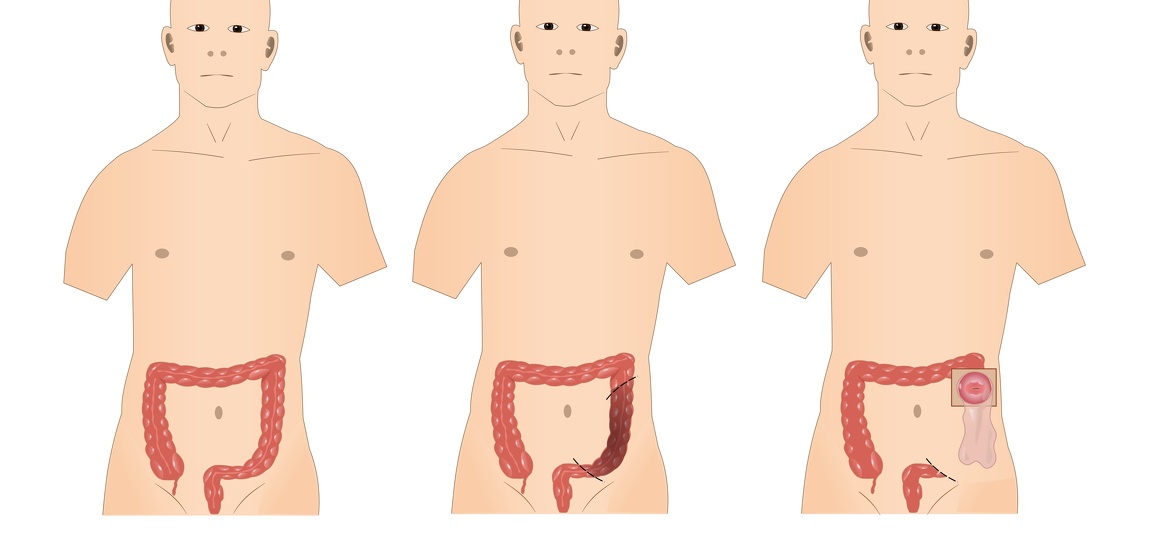
Surgery for IBD
What is ulcerative colitis?
Ulcerative colitis is a type of inflammatory bowel disease that happens when the lining of the rectum, colon, or both becomes inflamed. The inflammation produces tiny sores known as ulcers on the lining of the colon. It often starts in the rectum and spreads upward. Your bowel moves its contents rapidly and empties frequently due to the inflammation. When the cells on the surface of the lining of the bowel die, ulcers form. The ulcers can lead to bleeding, as well as the discharge of pus and mucus. Ulcerative colitis can be debilitating, and sometimes, it can lead to life-threatening complications.
Causes of ulcerative colitis
Like Crohn’s disease, the cause of ulcerative colitis remains unknown. Researchers believe that the condition may result from an overactive immune system. However, it is still unclear why some immune systems attack the large intestines and not others. Heredity also plays a role in the development of ulcerative colitis. It is found that the condition is more common in people with family members who have the disease.
While the cause is largely unknown, some factors can increase your risk of developing ulcerative colitis. These include:
- Family history – you may inherit a gene from a parent that has ulcerative colitis.
- Age – ulcerative colitis can strike at any age. However, it often begins before you are 30 or after 60. It occurs more often in older men than older women.
- Race or ethnicity – the condition can occur in any race, but whites, especially Ashkenazi Jewish descent, is at a higher risk.
- Environment – viruses, bacteria, and antigens in the environment may trigger the immune system. The use of antibiotics, birth control pills, and anti-inflammatory drugs may increase the risk slightly. A high-fat diet is also known to increase the risk.
Other things that can cause or trigger a flare-up are emotional distress, stress, and certain kinds of food.
Symptoms of ulcerative colitis
The symptoms of ulcerative colitis may vary, depending on where the inflammation occurs and the severity of it. The symptoms may also change over time.
Those diagnosed with the condition may experience periods of mild symptoms or no symptoms at all (known as remission). Nonetheless, the symptoms can return and be more severe (known as a flare-up).
The most common signs and symptoms of ulcerative colitis are:
- Diarrhea, usually with pus or blood
- Rectal pain
- Abdominal pain and cramping
- The urgency to use the toilet
- Inability to use the toilet in spite of the urgency
- Rectal bleeding (blood in the stool)
- Unexplained weight loss
- Fever
- Fatigue
- In children, failure to grow.
Ulcerative colitis can also cause additional conditions, such as:
- Joint swelling and/or pain
- Nausea
- Decreased appetite
- Skin problems
- Eye inflammation
- Mouth sores.
Complications of ulcerative colitis
Ulcerative colitis may complicate. Below are the complications of ulcerative colitis:
- A hole in the colon (perforated colon)
- Liver disease (rare)
- Inflammation of joints, skin, ad eyes
- Osteoporosis
- Severe bleeding
- A rapidly swelling colon
- Severe dehydration
- An increased risk of colon cancer
- Increased risk of blood clots in arteries and veins.
Diagnosis and Treatment of ulcerative colitis
To help confirm a diagnosis of ulcerative colitis, your doctor may perform one or more tests, including blood tests, stool samples, colonoscopy, flexible sigmoidoscopy, CT scan, and X-ray. If you are diagnosed with ulcerative colitis, you and your doctor will discuss your treatment plan.
The treatment for ulcerative colitis usually involves medication and surgery. The goal of treatment is to reduce the inflammation to prevent flare-ups.
- Medication
To reduce swelling and inflammation, your doctor may prescribe medication. The types of medication used may include:
- Sulfasalazine (Azulfidine)
- Mesalamine (Lialda and Asacol)
- Olsalazine (Dipentum)
- Balsalazide (Colazal).
In some cases, antibiotics, corticosteroids, medications suppressing immune function, or biologics may be needed.
- Hospitalization
If you experience severe symptoms, you will have to be hospitalized in order to correct the effects of loss electrolytes and dehydration that diarrhea causes. In addition, you may need to replace blood or to treat other complications. Researchers continue to look for new ulcerative colitis treatment.
- Surgery
Surgery may be necessary if you experience chronic symptoms, large blood loss, a severe blockage, or perforation of the colon. These serious problems can be detected by a CT scan. Surgery for ulcerative colitis may involve removing the whole colon and creating a pathway for waste. This pathway can be redirected back through the end of the rectum or out through a tiny opening in the abdominal wall.
